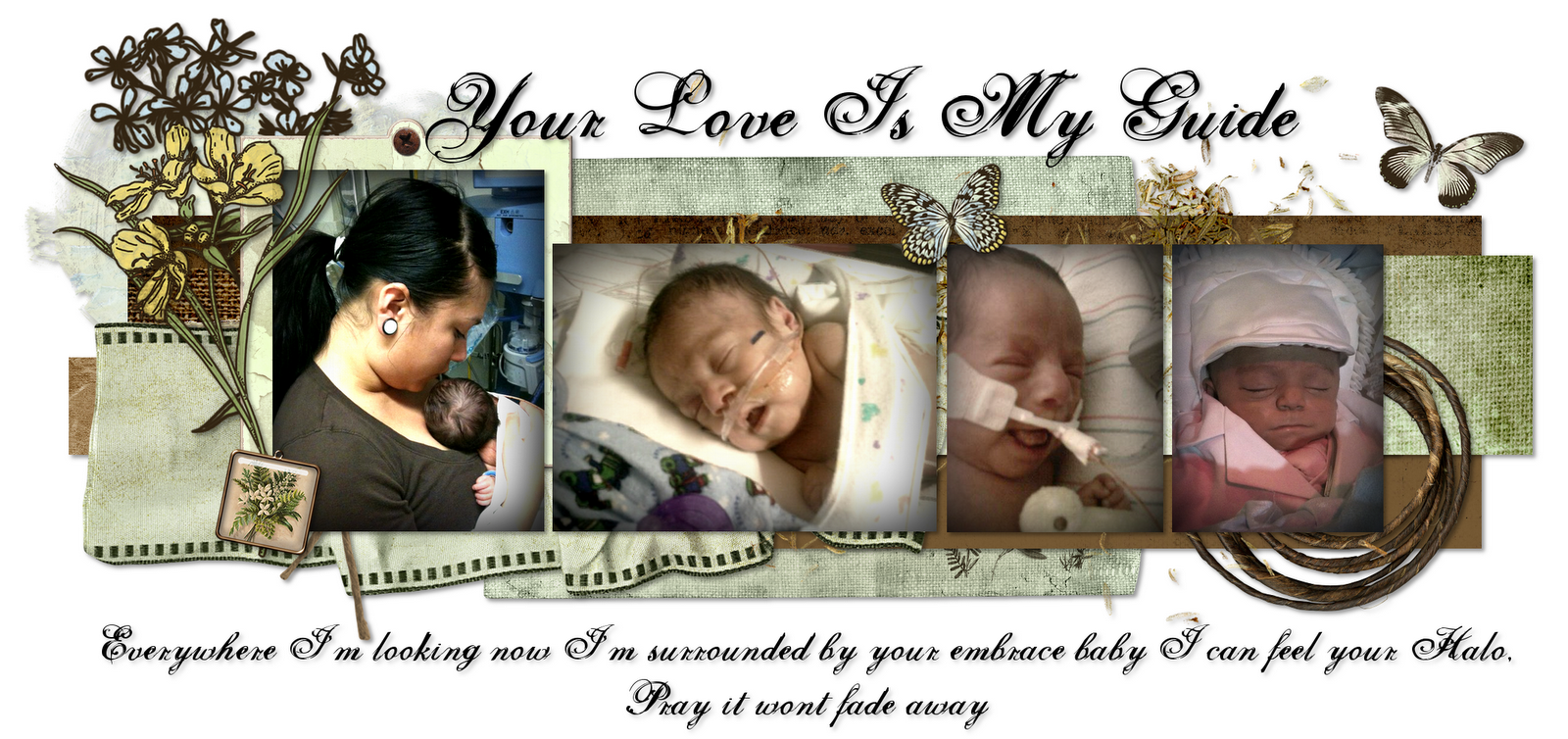
Mason continued to be well enough for me to carry him, on the 16th I was able to hold him for about an hour. He did start getting a little aggitated so we put him back down. They continued to increase his feeds and decrease his ventilator settings. It's kind of crazy how things could go from being stable to being critical.
The next morning when I called in for an update I wasn't really ready to hear that Mason was up to 100% his blood gases were going south and he needed to be placed on a high frequency ventilator...Here we were taking another 5 steps back. I remember asking God when this was going to end, for once in these 150 something days I was finally at my breaking point...How much more of this can we take, he gets better..he gets worse...I told God I couldn't do it anymore and that is something ill never forgive myself for even thinking, let alone screaming it out loud. I had been keeping composure for so long, trying to be strong...as strong as this little boy was being but I just was loosing all hope that I could one day raise my child. As soon as I went in that day I called his doctor to speak with him about the Trach. It was obviously something he needed and IMMEDIATELY! but would the surgeon go on with the procedure although Mason wasn't doing so well and on a high frequency?? I started writing down all the questions I had for the EENT.
His vent settings were going up, but why? later that day I found out it was not only an infection that was causing this but it was sepsis, an infection in the blood stream. We started realizing that Mason was worse off being in a hospital , he was being susceptible to all the nocosomial infections Hospitals carry. His poor immune system could hardly fight them. He was of course immediately started on antibiotics.
I met with the EENT and she told me she wouldn't be able to do anything until he was clear from infection but we did discuss maybe putting in Masons Gtube and possibly removing a hernia he had all at once just so that he didn't have to go through many different surgeries. She told me I had to get it cleared by his primary and by cardiology. I met with his doctors and they told me it was all up to Cardiology.
By the 18th Mason was actually getting better, his blood gases were starting to improve and his ventilator settings were going down too. I was starting to get a little more hopeful about actually going through with the surgery and finally getting over this pulmonary hypertension problem and finally get rid of being intubated. We scheduled the surgery for Friday May 28th. I frankly could not wait..This was the final step to finally being able to bring Mason home. Just 10 more days and we can finally move on..I couldn't wait.
I could tell he was starting to feel better because he was starting to become active again. He always spent a lot of time kicking his legs but when he didn't feel good he would sleep most of the day. On the 19th Mason was switched from a high frequency vent back to a regular vent and restarted on his PO medications. I felt horrible for doubting in God like that...I remember going to the chapel that night and really asking for forgiveness, he had once proven me wrong...Everything was falling into place again. And we were back on track....or so we thought.
It's in his heart
8 years ago