Mason continued to be on the road to recovery, I didn't know how it was possible really. My baby had just overcome not only a Chylothorax but a Pneumothorax which both together alone should have killed him. One of the nurses had told be a few days back that they had never had a baby survive a Chylo, that was when I pretty much lost hope. Although Mason would constantly get critically ill for some odd reason I was never too alarmed, I guess because he had overcome so much that I thought he was capable of anything. But this last time, when I saw all the drainage I just didn't think he'd survive. But here we were, once again on our way back to actually taking steps forward. They continued to lower Mason's respiratory settings which was always a good sign. He was still on a high frequency ventilator but was on much lower settings, low enough that they could possibly change him over to a conventional ventilator any day now.
On May 3rd they ordered an Echo just to make sure that his pulmonary hypertension was under control throughout all the mayhem he had been through the last 2 weeks. He still had one chest tube but it was practically not draining anything, maybe a cc an hour. I emailed Dr B to ask if he would do an Xray before removing that chest tube. He said said he would order it and come see Mason the following day.
The following day Dr B came in and took the second chest tube off. He also discontinued the Octreotide. This was a huge deal for us, I didn't know how to thank this doctor who had saved my babies life plenty of times before. He told me he would continue to monitor him. I couldn't hold Mason on a Osscilator (high frequency vent) because it was giving him too much pressure to move him, But I could hold him once he was switched over to the conventional. Little did I know that they were going to switch them over that night. Part of me felt a little hesitant, what if this was pushing him too much too fast. After all he had just gotten through a lot. But Doctors knew best and I always put my thrust in the team I picked out for Mason. His first blood gas which checked his respiratory status, was good. I was a bit relieved and very surprised that even after all of this Mason was requiring very minimal blood pressure support.
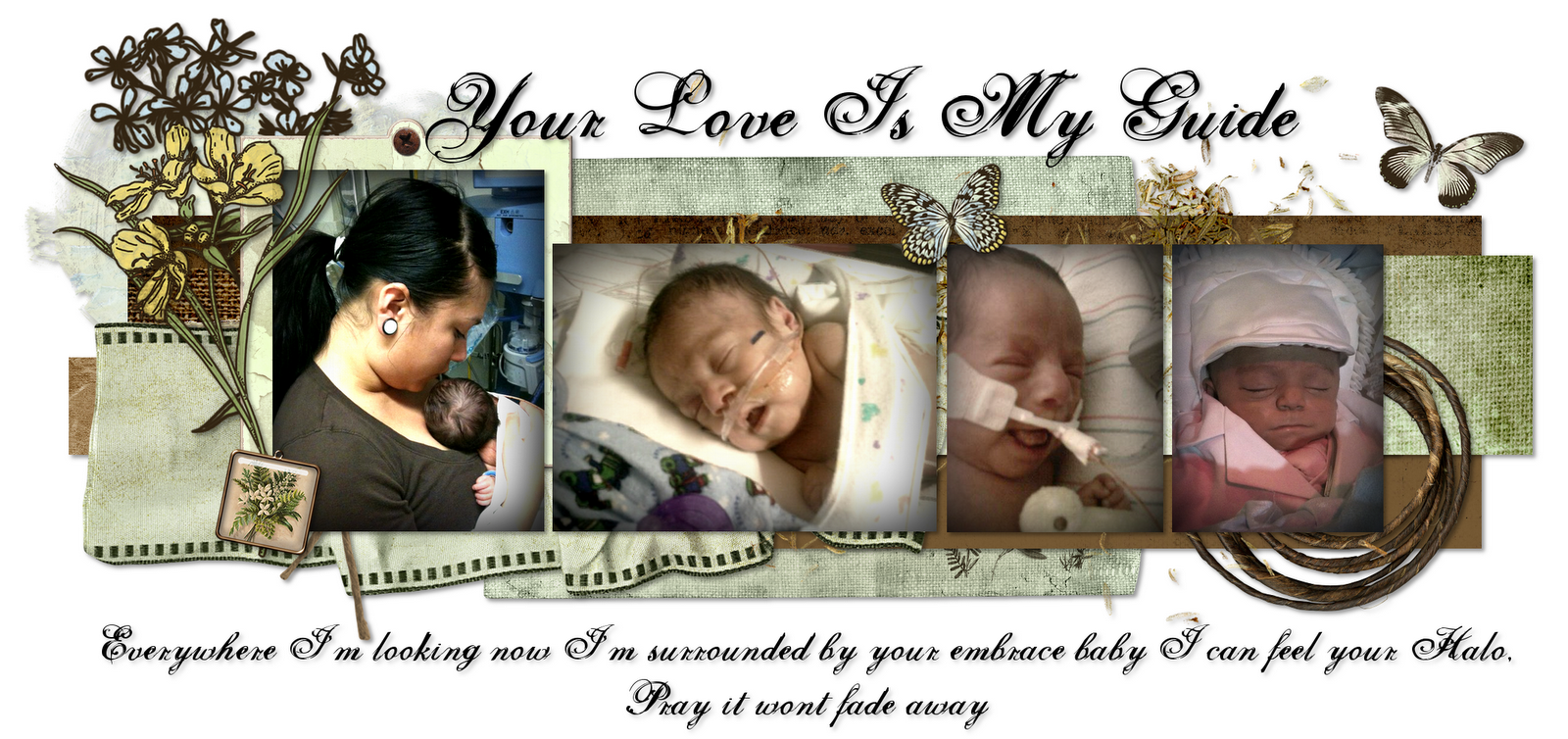
The days went by and Mason seemed to be on the right track, by May 10th which was my first Mothers day with my child, I was able to actually hold Mason I spent some time at a BBQ we had with my mom at home and at around 2 I headed to Millers. As soon as I got there me and Jenna started his feed and we prepared for me to hold him. I remember holding him for 2 hours straight, until my arms pretty much gave up. I loved cherishing moments like that with him, he fell sound asleep.
The next day Mason decided to extubate so they tried him on CPAP but he did not tolerate it so they re intubated him and we started discussing a trach. At this point we were pretty certain that Mason was going to need additional breathing help for a while, he had just endured too much damage with all those extubations that it was going to take a while for his lungs to recover and a trach was probably the best decision for him. The next day his dad came and visited with me and he got to hold Mason for probably the 3rd or 4th time in Masons life, Louis was afraid of carrying Mason so he hardly ever did, I was the one who would hold him and he would just watch. At this point I was working from 8-2 and then visiting Mason the rest of the day. It was much better than working 8-6 and then visiting Mason until 10 pm. Those days were very long and very draining. I would constantly argue with him and ask him why this was all put in my hands, Before Mason I had no medical experience everything I knew was because i was on top of his care. But I was literally the one in charge of making every life changing decision and it bothered me a lot. We were supposed to be a team and he was supposed to help with everything, not just be there. That day Louis held Mason for a while, the longest Louis had probably ever held him; it would also be the last.
I wanted to see what was next in Masons care plan so I arranged a meeting with his Doctors. We discussed how evidently Mason was not succeeding at extubating and that we needed to come up with a better solution. We discussed the Trach and agreed that i would go meet with the ENT (ears nose and throat). In the meanwhile they were increasing his feeds and lowering his vent settings.This was the first 2 weeks of May and we were not prepared for what was about to happen.
It's in his heart
8 years ago























6 comments:
<3<3<3
your son is gorgeous...I can not imagine what you went through. I know I lost a child, but it was different. Your heart was literally tugged ALL the time...seeing him go up and then down and then up again...doing this while working, and with a husband who wasnt 'there' for you....Im praying for you Karen because that is all i can do from all the way over here...but If i was closer I would hug you as hard as I could and hope that I squeezed some of the pain out....I love you and im so sorry mason and madison are not HERE with you...xoxo...
;q
=( this is sad, ur such a strong women, to write about it an re tell all u went through must of been hard remembering it all over again <3
Tough like Mommy! :) Prayers & God Bless <3
God Bless You.
Post a Comment