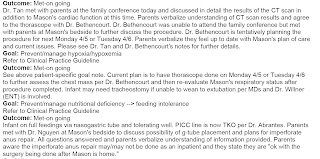
Mason seemed to be recovering well from surgery, he was draining very little and Dr. B wasn't too concerned as long as we were replacing, by the 5th they had restarted his feeds. This was one thing I hated abut us taking steps back, we had already gotten to full feeds and we would have to start slow again but luckily not from the beginning they were starting at 10ml's over 3 hrs. This means he was getting about an oz every 3 hours which wasn't too bad. I had not been able to hold my baby since the 2nd when we had the family conference and before he was taken to the PICU for surgery and I was starting to get anxious. I knew I couldn't hold him while he had a chest tube, that would just be too painful. But he was waking up, although you can clearly tell he was in pain.
By the 7th Mason was getting worse, he began draining a lot of fluid from his chest tube, so much that they were not replacing it every 6 hrs but every 3 hrs. Once they talked to Dr B. He suggested to start Mason on a medication called Octreotide because he suspected Mason could have a Chylothorax since they sent the fluid he was draining to the lab and it came back with a high triglyceride level which meant it was coming from the thoracic duct. What most likely happened was that when he went in for the exploratory thorascope he probably punctured the thoracic duct which was now draining more than it should. I talked to Dr. B and he said that the octreotide would help close it without him having to go in but that this medication could take weeks to make a difference. He told me he would monitor him and in the worst scenario he would have to go in and do a thoracic duct ligation which meant yet another surgery.
By the 10th of April Mason went from draining about 40 to 50 cc's to about 200 cc's every 12 hours. They had already increased the chylothorax medication to the highest they could but it was not working, Mason was continuing to go downhill, On the 10th they placed him on a high frequency ventilator called an oscillator. This would help him breath as they wanted to keep him as comfortable as possible. We did not only have to worry about the chylo but also infections, he was susceptible to getting an ET infection a chest tube infection, a PICC or IV line infection. When his respiratory status went south we more than likely knew there was some sort of infection setting in so they immediately started him on antibiotics. The morning of the 13th Dr. B called me and told me he was going to take Mason up to the Cardiology unit to do the Thoracic ligation. I rushed to the hospital to see him before he went in yet again, this would be the 4th time they opened him up to see what was going on. Dr. B did the ligation and Mason returned with 2 chest tubes
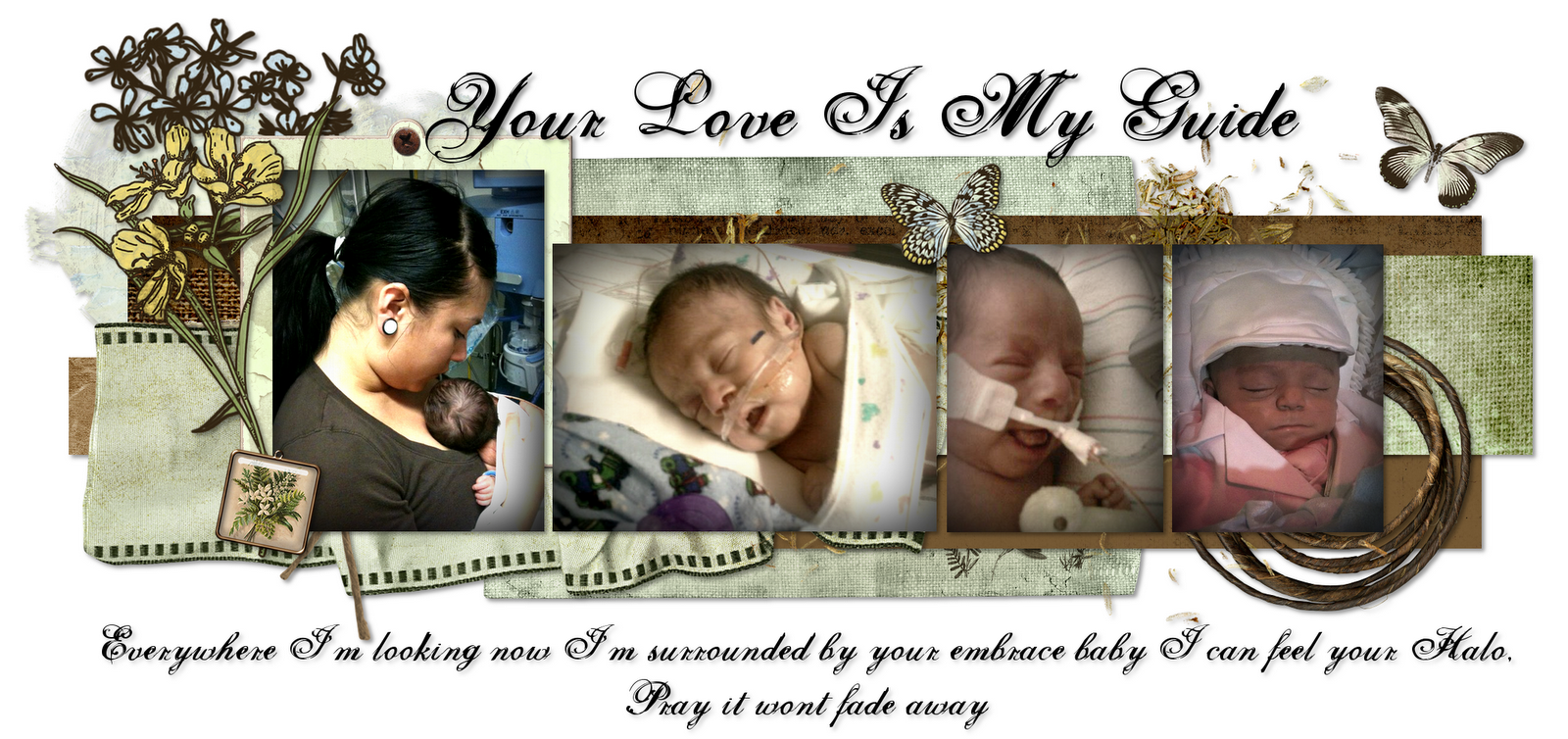
When Mason came out of surgery he wasn't in a very stable condition, he was at 100% oxygen and his saturation's were not in the 90's where they wanted them so they started him on INO to help with his breathing as well as with the pulmonary hypertension. Because of all this Mason was diagnosed with Chronic Lung disease. This was a very tough time because he was already on ALL the support they could give him yet he would still desat requiring them to bag him manually. All this was very hard to take as I had never seen my baby in such a critical condition. This was when we had a nurse tell us that she would not keep her baby like this and would DC respiratory support. I was very angry at the fact that she "A NURSE" could give me such advice. The next day his primary was in and I discussed this with her and she was appalled since Mason was actually getting better, They had lowered his INO from 10 to 5 and his oxygen from 10% to 75% and his output was lowering. I was optimistic and was not going to give up on my baby just yet. Not even when they told me that NO baby had ever survived a chylothorax in their unit. This was the beginning of April, a very bad month for Mason.
















































0 comments:
Post a Comment