Mason was recovering really well from surgery, for the past week he had been draining extra fluid through his chest tube so they had been replacing it with albumin. He was having some fluid imbalances so they had to start replacing what he was draining. He had been switched from the high frequency to the regular ventilator but was still on Nitric Oxide to help with the mild pulmonary hypertension issue we were having as well. This was the first time Mason showed signs of pulmonary hypertension. It had been over 2 months and he had continuously been intubated. If there was something I couldn't wait for was for that tube to come out, he was sick of it and it hurt me so bad. He would constantly pull and yank it. It hurt to see my baby aggitated because he was in pain, other than an incision he had a chest tube..I don't know if you've ever had a chest tube but I hear it is one of the most painful things. They were doing a great job at keeping him relaxed and it took a few days but he slowly stopped draining and the chest tube came out, He seemed a lot happier once the chest tube came out, We were on the road to recovery from here.....On the 12th he extubated himself and for the first time they tried him on CPAP, he didn't tolerate it so he was intubated about 30 minutes later. When I heard this I was devastated, He wasn't ready what if he could never adjust? Was it because he was just recovering or was it because he needed another 2 months to try. If he didn't tolerate it now then when would he? was he still not fully recovered? After all it had only been 10 days after surgery. He needed a little more time. I had all the faith in the world in Mason. They were soon going to push him to try and extubate and if it didn't work than what would be next? They were slowly weening on his sedation and ventilator settings as he was able to tolerate. This meant he would have to wake up and try the breathing on his own, with no ventilator help. He had been NPO up until the 15th when they restarted his feeds. This was a huge step for us but we were going to have to start from the bottom and work ourselfs up. They would try and push him but would be cautious. His blood pressure was stable and he was off all pressors except for Soluf Cortef which he was receiving every 12 hours, they would wean that as he tolerated it too. He was restarted at 5ml for 6 hrs straight which is an oz given at 5ml an hr. He would get increased as he tolerated it.
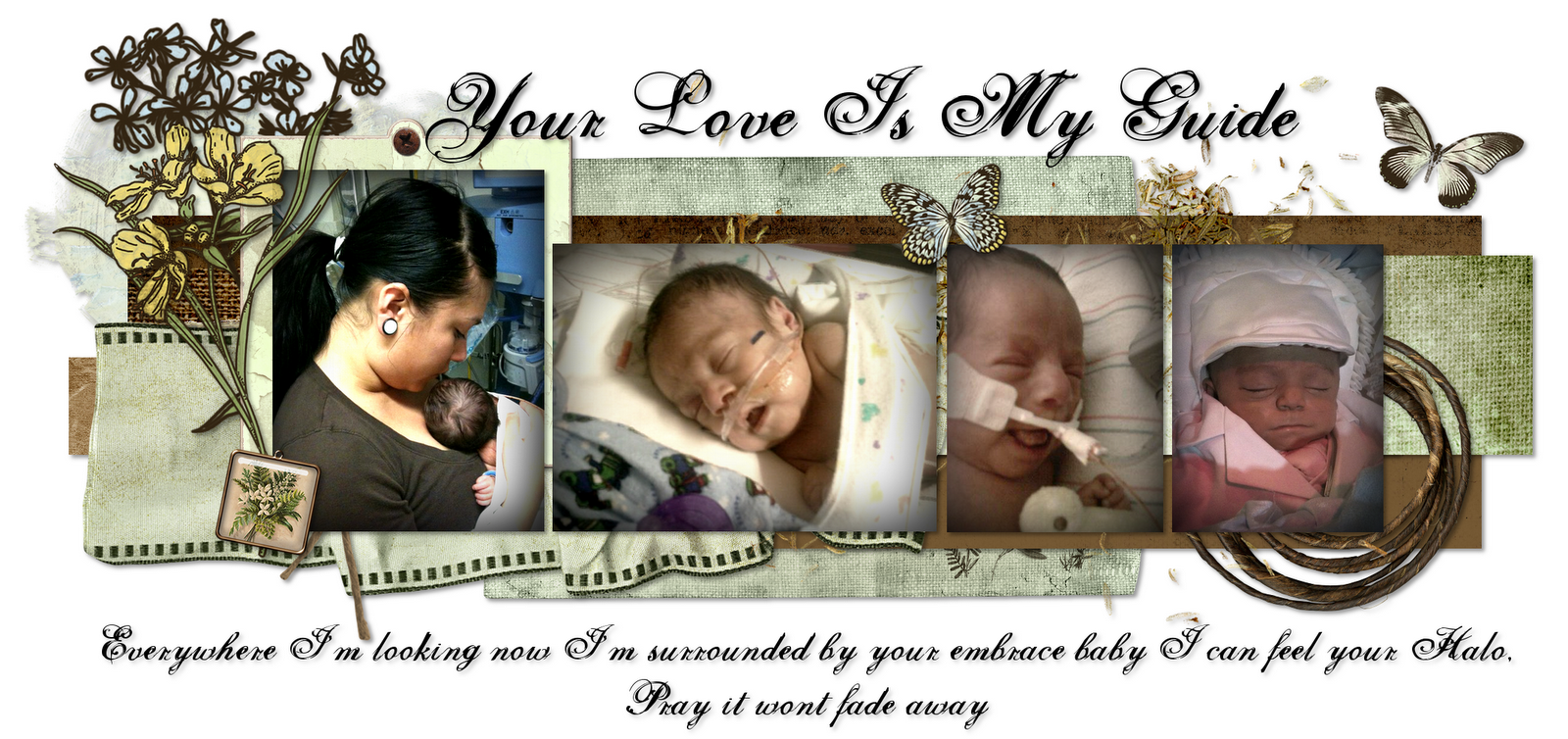
The morning of the 15th I called Jenna in the morning and she told me that Mason had once again extubated and that she was trying him on nasal cannula and that he was tolerating it pretty well, he was keeping the desired saturations and he was only on 50% oxygen. I was more than thrilled to hear this but i asked her if she thought he would last. She told me we would wait and see but that he was going to get some help with a dose of stereroids. I was a little more convinced after I heard that he would be receiving help. She also told me that if he didnt tolerate cannula well there was always cpap and sipap which could be a little more easier on him but they wanted to push and see if he can just handle the cannula. I had never seen my baby off the ventilator and this got me so excited i left work early and told them I had to go talk to a doctor. I got to the hospital to see my baby's beautiful face for the first time with no tube.
The cannula only lasted 2 days by the 19th Mason had been placed on Sipap. Me and Jenna discussed it and we realized that Mason was going through a big change in sedation medication and he was slowly starting to do all the work himself breathing. Since he had been on medications that were really strong for a very long time his body was use to them and it was going to take a while for his body to slowly get use to it. Its like any drug you take, your body relapses after they just start taking it away. It got so bad he would get so aggitated that they decided to start him on methadone, we were getting rid of fentanyl but we would be introducing methadone. I knew it was going to be hard work to get Mason on the road to recovery but I never imagined it would be this hard. We literally took 1 step forward and then 3 steps back. I was enjoying the time that Mason was not intubated because I could just hold him when ever I wanted. The Sipap lasted till the 24th, Masons blood gases went so bad that they had to re intubate him.
I got to the hospital as soon as they were re intubating him so I got to talk to the doctor, he told us his chest Xray showed pulmonary edema and due to my baby looking so pale and tired they decided to to an echo which showed an enlarge heart, this could be due to him working so hard to breath on his own or the pulmonary edema. His tummy was also really bloated, they felt his stomach might need to be ventilated since he was on Sipap and Mason did not know how to control not sucking so much air in. All this together plus pulmonary hypertension resulted in him having to be re intubated. I had also talked to the GI surgeon which informed us Mason would not have his pull through during his hospital stay, they would wait atleast a year for him to get a little bigger and do it as an outpatient procedure.I didnt mind this at all, this meant I would take my baby home with a colostomy which I did not mind. I knew how to change it and care for it so it was not much of a big deal.
I knew it was a long road to recovery, but never imagined it to be so long. We still had a lot to come Mason was also full of surprises he could get better from being real sick, or get real sick after being compleatly fine. That was my boy, very unnexpected. He kept us on our toes his whole life, this was February and we were pretty much recovered from surgery.
It's in his heart
7 years ago

















































0 comments:
Post a Comment